Plastics possess many unique properties, can be used to make many different products and are highly manufacturable. These properties are being increasingly exploited in the production of medical packaging and devices.
The medical device sector is one of the fastest growing sectors for plastic use, exceeding the growth rate of plastics in domestic products for some years now. It is expected that this trend will continue as more and more innovative medical devices and produced, populations continue to age and plastic processing and materials continue to improve.
Whilst there are currently many changes taking place in the industry there is one thing that has remained the same – materials in medical devices must adhere to strict safety guidelines.
Biocompatibility
Biocompatibility describes how suitable a material is for inclusion in the body, or for exposure to bodily fluids, without causing a negative host response. The biocompatibility of a material depends on the specific application that it will be used for, meaning a material could be biocompatible for one application but not for another.
Generally speaking a material would be thought of as biocompatible if it causes no negative impact to the host for the application being considered. It should be noted that this excludes side effects and other consequences; with some biocompatible materials still resulting in immune and inflammatory responses. However, if the material is biocompatible these responses should not cause harm and are part of normal body function.
Non-biocompatible materials will cause damaging effects to the host; where they can interrupt healing processes or result in more severe consequences. Indications that a material is not biocompatible include:
- The production of cytotoxic compounds
- Thrombosis, i.e. the formation of blood clots
- Chronic inflammation at the site of contact
- Skin irritation
- Cell disruption
- Restenosis, i.e. narrowing of blood vessels following stenting
- Corrosion of the material
The severity of these consequences demonstrates that biocompatibility is a key barrier that potential implants and devices must find a solution around.
Testing and Assessment
The testing methods used to evaluate the biocompatibility of a material vary widely depending on the intended application of the material, with some tests not being required for certain applications.
There are many different possible testing methods, with in vitro and in vivo methods available. Testing methods examine properties such as hemocompatibility, cytotoxicity, genotoxicity, system toxicity, sensitization, irritation and implantation. The testing methods used must also consider the possible misuse of the material or device being tested.
ISO 10993: Biological Evaluation of Medical Devices
The International Organization for Standardization (ISO) provides well recognized guidelines for medical devices that aim to mitigate risk. ISO standard 10993 is concerned with biocompatibility testing. There are also other country-specific bodies which overlap with this regulation but they will not be discussed in this article.
ISO standard 10993, titled “Biological evaluation of medical devices”, has twenty sections (at the time of writing) and is updated regularly to accommodate new discoveries (Table 1). The first step in the testing of biocompatibility involves looking at the material being used and, if the material has an established history of working in medical contexts, this testing step can be skipped. If the material used is novel or has no established medical history then ISO 10993 can guide users on how to properly test it.
Table 1. Structure and parts of ISO 10993: Biological evaluation of medical devices
| Part |
Title |
| 1 |
Evaluation and testing |
| 2 |
Animal welfare requirements |
| 3 |
Tests for genotoxicity, carcinogeniticity and reproductive toxicity |
| 4 |
Selection of tests for interaction with blood |
| 5 |
Tests for cytotoxicity - in vitro methods |
| 6 |
Tests for local effects after implantation |
| 7 |
Ethylene oxide sterilization residuals |
| 8 |
Clinical investigation of medical devices |
| 9 |
Degradation of materials related to biological testing |
| 10 |
Test for irritation and sensitization |
| 11 |
Test for systemic toxicity |
| 12 |
Sample preparation and reference materials |
| 13 |
Identification and qualification of degradation products from polymers |
| 14 |
Identification and qualification of degradation products from ceramics |
| 15 |
Identification and qualification of degradation products from coated and uncoated metals and alloys |
| 16 |
Toxicokinetic study design for degradation products |
| 17 |
Glutaraldehyde and formaldehyde residues in industrially sterilized medical devices |
| 18 |
Chemical characterization of materials |
| 19 |
Physico-chemical, morphological and topographical characterization of materials |
| 20 |
Principles and methods for immunotoxicology testing of medical devices |
The test program to use is determined by the category that the device is classified in by ISO 10933. Classification into these categories uses parameters such as the material being used, how the device will contact the body, and how long for (Table 2).
Table 2. Device categories and biological evaluation of medical devices for ISO (from ISO 10993: Part 1).
| Device category |
Contact regime |
Contact Timescale |
Example products |
| Surface devices |
Skin
Mucous membrane
Breached or compromised surfaces |
Limited
Prolonged
Permanent
Limited
Prolonged
Permanent
Limited
Prolonged
Permanent |
Electrodes, external prostheses, fixation tapes, compression bandages, monitors of various types
Contact lenses, urinary catheters, intravaginal and intraintestinal devices (stomach tubes, sigmoidoscopes, colonoscopes, gastroscopes), endotracheal tubes, bronchoscopes, dental prostheses, orthodontic devices, IUDs
Ulcer, burn and granulation tissue dressings or healing devices, occlusive patches |
| Externally communicating devices |
Blood path indirect |
Limited
Prolonged
Permanent |
Solution administration sets, extension sets, transfer sets, blood administration sets |
| Tissue / bone / dentin communicating |
Limited
Prolonged
Permanent |
Laparoscopes, arthroscopes, draining systems, dental cements, dental filling materials, skin staples |
| Circulating blood |
Limited
Prolonged
Permanent |
Intravascular catheters, temporary pacemaker electrodes, oxygenators, extracorporeal oxygenator tubing and accessories, dialyzers, dialysis tubing and accessories, hemoadsorbents and immunoadsorbents |
| Implant devices |
Tissue / bone implant Devices
Blood |
Limited
Prolonged
Permanent
Limited
Prolonged
Permanent |
Orthopedic pins, plates, replacement joints, bone prostheses, cements and intraosseous devices, pacemakers, drug supply devices, neuromuscular sensors and simulators, replacement tendons, breast implants, artificial larynxes, subperiosteal implants, ligation clips
Pacemaker electrodes, artificial arteriovenous fistulae, heart valves, vascular grafts, internal drug delivery catheters, ventricular assist devices |
| Time Span Key: |
Limited: < 24 hours |
Prolonged: 24 hrs - 30 d |
Permanent: > 30 days |
The device can contact the body through different regimes such as bone, blood, skin, or more. The contact time is broken down into three categories – permanent (more than 30 days), prolonged (24 hours to 30 days) and short-term (less than 1 day). Considering these different factors helps manufacturers determine how to test the biocompatibility of their device.
ISO 10993 is not itself a formal checklist for manufacturers to work through, but is instead a guide to understanding the requirements to have a device approved; helping manufacturers carry out the right testing for their product. For this reason, the details of tests are specific to different types of applications and devices, though there can be crossovers.
Testing details are thus specific to each device and its application, though there may be testing commonalities for multiple device types.
Other Regulations
Alongside ISO 10933, the Food and Drug Administration (FDA) of the USA also regulates medical devices. The guidelines set by the FDA tend to correspond to ISO 10993 regulations, meaning the results for ISO tests can often be used for USA applications.
Devices for use in the EU must adhere to regulations set by the European Commission; with (EU) 2017/745-6 covering medical devices (including in vitro diagnostic devices).
As a whole these different regulatory bodies can cover nearly all concerns with medical device testing. For more information on specific types of tests please see the relevant sections of ISO10993, or the EU or FDA regulations.
United States Pharmacopoeia (USP)
In some sectors the USP has been made redundant by ISO 10993 for medical device testing; however, some manufacturers still work by USP standards.
One of these examples is in vitro biological reactivity tests (USP 88), which is a method used to measure how animals respond to plastics either by indirect contact, direct contact or following injection with the plastic. These tests can involve implantation, intracutaneous exposure and systemic injection (intravenous and intraperitoneal). The test used depends on the application and contact area for the plastic component being tested.
The methods used for administration are also defined by USP 88. For example, intracutaneous tests and systemic injection tests use extracts that have been prepared at either 121 °C (250 °F) for 1 hour, 70 °C (158 °F) for 24 hours or 50 °C (122 °F) for 72 hours. Different types of media (such as ethanol, saline, cottonseed oil or polyethylene glycol) are also part of USP 88 testing.
USP 88 is used to determine how biocompatible a plastic is, classifying them on a scale between class I and class VI.
Material Characterization
Being able to comprehensively characterize a material is an important requirement for the determination of a material’s biocompatibility. This characterization involves mechanical, chemical and thermal testing (Figure 1).
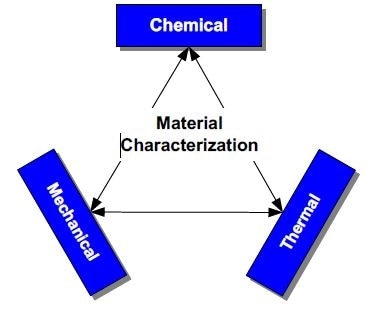
Figure 1. Elements of material characterization: mechanical, thermal, and chemical.
The characterization of plastics is especially important as similar grades of plastic can show widely different chemical and physical characteristics; with the different additives used during plastics manufacturing (such as fillers, stabilizers and plasticizers) all impacting biocompatibility.
Plastics with additives must be analyzed using leaching studies to ensure that no toxic compounds leach from the plastic. The type of additive used, and in what volume it is added, has an impact on how biocompatible a plastic is.
Chemical Testing
The chemical testing used to characterize materials can take place using several different techniques that all look at different material aspects. Such tests can include extraction analysis, infrared (IR) analysis, trace metal analysis, and gas or liquid chromatography.
Extraction analysis is used to determine if any substances leach from the material. IR analysis provides qualitative and semi-quantitative information on the constitution of the material. Trace metal analysis is used to determine if any trace toxic metals (e.g. lead, barium, tin, bismuth, etc.) remain present from processing of the material. Chromatography is used to determine if additives are present, and if there are any degradation products or leftover monomer from polymer production processes.
Chemical testing gives manufacturers insight into how their materials, and the devices produced from them, will behave in the body and if this will impact human safety.
Mechanical Testing
The mechanical performance requirements of a medical device depends on the application it will be used in; with the device performance itself limited by the materials used to construct it.
Mechanical testing is necessary to determine if the behavior of the material (i.e. tensile strength, toughness, stress-strain behavior, elasticity, and more) is adequate for the application of the finished device. Mechanical failure is of as great a consequence as issues with biocompatibility, meaning correct testing is important. In addition, whilst mechanical factors do not directly impact biocompatibility, mechanical testing allows materials which will perform the best in a specific application to be chosen.
Thermal Testing
Thermal testing is carried out to assess a plastic’s response to heating. Techniques such as differential scanning calorimetry (DSC) and thermogravimetric analysis (TGA) are two common test methods employed for biocompatibility thermal testing. TGA measures the test material’s change in weight as it is heated. DSC compares the temperatures of a reference material and an unknown (test) sample as they are heated.
Thermal tests provide important information on the material being tested such as its thermal history, phase structure, purity, glass transition temperature (Tg) and melting point (Tm). This information helps manufacturers decide how viable a material is for use in a medical device or component.
Sterilization
The impact of sterilization on a material should also be considered in addition to its biocompatibility. All medical devices must be sterilized before coming into contact with the body and this can place stress on the material.
Single use devices must only survive one sterilization however multiple use products must be able to survive multiple sterilizations, and may be exposed to many different sterilization methods over their lifetime.
Biocompatible materials must be able to survive sterilizations without losing their useful properties or breaking down significantly. For this reason, the impact of sterilization should be determined early in the materials evaluation process.
Biocompatible Plastics
Pure plastics tend to be chemically inert meaning they are appropriate for applications involving bodily contact. However, variations of plastics may not show the same biocompatibility, or native versions may not be appropriate for more demanding biological environments.
Plastics such as PEEK and PTFE are extremely chemically inert making them popular medical materials. Other plastics have other wide-ranging biocompatible properties which makes them popular for use in less critical applications (Table 3). New plastics are always in development that can complement old plastics, or even replace them entirely.
Table 3. Selected plastics and their common biomedical applications
| Plastic family |
Typical applications |
| Polycarbonate (PC) |
Dialysis filter cartridges, highly transparent glass containers, tubing and intravenous (IV) connectors, component for blood oxygenators, trocars |
| Polyetheretherketone (PEEK) |
Prostheses, dental products, rigid tubing, replacements for metal implants |
| Polyethersulfone (PES) |
Membranes: hemodialysis, gas separation, others; tubing, catheters, implantable drug infusion device |
| Polyethylene (PE, of various types) |
Implantable products, sutures, surgical cables, orthopedic, and artificial tendons, catheter inner lining |
| Polypropylene (PP) |
Suture material, meshes, laboratory containers and tubes, drug delivery systems |
| Polysulfone (PS) |
Implantable ports, dialyzers, surgical instruments, device housings |
| Polytetrafluoroethylene (PTFE) |
Vascular grafts, suture material, catheter base liners, prostheses |
Polyurethane (PU)
Polyvinylchloride (PVC) |
Artificial hearts, wound dressings, catheter tubing, surgical drains
Blood bags, feeding tubes, catheters / cannulae, inflatable splints |
| Polyetherimide (PEI) |
Machinable parts for reusable medical devices, IV sets, medical and dental instruments, pharmaceutical containers |
Fluoropolymers and Biocompatibility
One of the most biocompatible types of plastic are fluoropolymers, and for this reason they are widely used throughout the medical industry. Fluoropolymers tend to be alkene based and have many favorable properties such as chemical inertness within the body, a high lubricity, a wide temperature tolerance, ease of sterilization, and (most importantly) biocompatibility.
Fluoropolymers that are Class VI USP approved include PTFE, ETFE, FEP, PFA and PVDF (to name just a handful). Due to their favorable properties fluoropolymers tend to be a good starting point when beginning to think about what plastic to use in a medical device.
Summary
Biocompatibility is a wide term that covers how appropriate a material is for use in applications involving bodily contact. Whilst implantable materials will almost always result in immune or inflammatory responses if a material is biocompatible these responses will not reach harmful levels.
The classification and testing of biocompatible materials are mostly based on guidelines such as ISO 10993, Regulation 2017/745-6 (EU), FDA regulations (USA), and the USP. The classification system used by the USP for plastics has classes I-VI, defined on how they perform in tests, with fluoropolymer-based fluoroplastics in Class VI.
Material evaluations of biocompatible plastics involve thermal, chemical and mechanical testing, in addition to sterilization testing; with most medical devices having to withstand many sterilization cycles.
Fluoropolymers are a popular material group for medical devices due to their attractive properties; including chemical and thermal inertness and high lubricity. It is not realistic to expect fully definite results from testing despite the established knowledge on the behavior of materials and the comprehensiveness of the tests used. Biocompatibility testing is a method of characterization based on current knowledge using the best available judgment.

This information has been sourced, reviewed and adapted from materials provided by Zeus.
For more information on this source, please visit Zeus.