3D printing is common in professional and academic laboratories as researchers discover innovative uses. Its central function is to quickly create complex 3D structures with great precision. The technology is now well integrated into multiple industries, such as chemical engineering, life sciences, materials science, and electrical engineering.
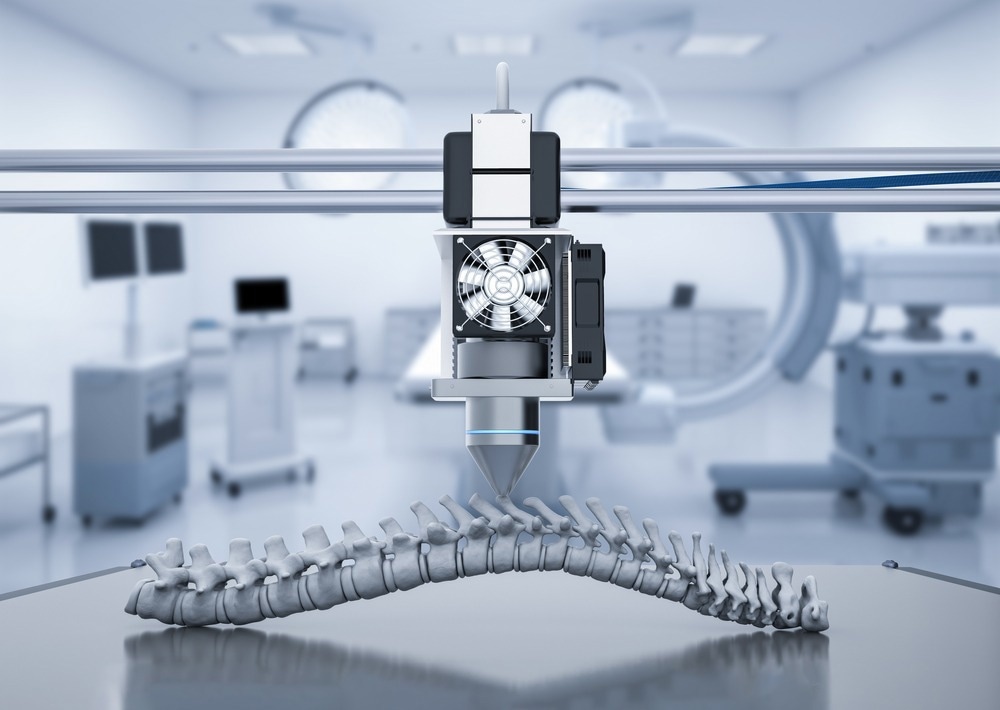
Image Credit: Phonlamai Photo/Shutterstock.com
Surface chemistry is crucial in all stages of 3D printing, from ink manufacturing to deposition and then processing. Plasma treatment is commonly used in combination with 3D printing to fine-tune surface chemistry at each stage. The main benefit of plasma is its even coverage of exposed 3D structures. It is also faster and simpler than many wet chemistry techniques. Plasma develops at ambient temperature and is not hazardous, maintaining the reliability of treated materials.
Harrick Plasma Cleaners are utilized to create many 3D-printed devices, including microfluidic devices, prostheses, 3D-printed organs, and bottlebrush block copolymers.
Microfluidics
With 3D printing, microfluidic device components can be built directly or indirectly by printing PDMS molds.
3D printing of microfluidic devices is a somewhat new channel, with recent improvements in resolution allowing microchannel printing. 3D printing can now be used to quickly prototype cell imaging devices, organ-on-a-chip systems, and cell culture environments.
While microfluidic devices are most commonly PDMS and glass-based, researchers have also used a variety of thermoplastics. For example, biocompatible materials like poly(ethylene glycol) diacrylate (PEGDA) resin can offer a more optimal cell culture environment.
Plasma cleaning is a critical step in the fabrication of PDMS microfluidic devices, as it facilitates 3D printing and allows watertight bonding of PDMS to glass or PDMS to PDMS.
Tissue Engineering and Disease Models
3D-printed biomimetic organs or tissues are disease models for developing drugs and treatments. It is especially beneficial because it can precisely recreate an organ's complex geometry.
In vitro experiments that use scaled-down models of human organs are less cumbersome and can result in more information than experiments that use animal or cellular disease models. In addition, 3D-printed drug testing systems are a possible alternative to animal testing. Harrick Plasma Cleaners render 3D-printed organoids hydrophilic to mimic the body's hydrophilic environment.

Image Credit: Scharfsinn/Shutterstock.com
3D-printed bioreactors are also useful in modeling the human body and introducing dynamic characteristics like media delivery and shear stress. Polycaprolactone (PCL) scaffolds are plasma treated to be hydrophilic before being introduced into 3D-printed bioreactors. These hydrophilic scaffolds are capable of supporting kidney cell survival and growth and allow the creation of scaffolds that are more standardized in comparison to conventional methods. These scaffolds in 3D-printed bioreactors function as tissue engineering tools as well as disease models for drug development.
3D printing is not just for internal organs. 3D-printed maxillofacial prostheses are under study as an alternative to the traditional method of production, which requires a lot of labor and limits who can access these prostheses.
Drug Delivery
3D printing can also be utilized in the development of drug delivery methods. 3D-printed miniaturized needle arrays (MNAS) were recently incorporated into the blueprint of a transdermal drug delivery patch. Plasma treatment was significant in attaching the needle arrays to the polydimethylsiloxane (PDMS) patch.
Composite Polymers
Another use of 3D printing is the building of composite polymers, which have applications in very conductive materials and color-tunable patterned photonic crystals. Plasma cleaners are useful in treating the substrates where the composite polymer printing process happens, typically silicon wafers. Plasma-treated silicon wafers are hydrophilic, which improves 3D printing of bottlebrush block copolymers (BBCPs).
References and Further Reading
Microfluidics Devices and 3D Printing: Articles by Harrick Plasma Users
- Su W, Li Y, Zhang L, Sun J, Liu S, and Ding X. “Typography-Like 3D-Printed Templates for the Lithography-Free Fabrication of Microfluidic Chips”. Sage Journals 2019 25: 82-87. 10.1177/2472630319867903
- Tsuda S, Jaffery H, Doran D, Hezwani M, Robbins PJ, Yoshida M, and Cronin L. “Customizable 3D printed ‘plug and play’ millifluidic devices for programmable fluidics”. PLoS One 2015 10: e0141640. 10.1371/journal.pone.0141640
- Linden PJ, Popov AM, and Pontomi D. “Accurate and rapid 3D printing of microfluidic devices using wavelength selection on a DLP printer”. Lab on a Chip 2020 20: 4128-4140. 10.1039/D0LC00767F
- Kadilak AL, Rehaag JC, Harrington CA, and Shor LM. “A 3D-printed microbial cell culture platform with in situ PEGDA hydrogel barriers for differential substrate delivery”. Biomicrofluidics 2017 11: 54109. 10.1063/1.5003477
- Warr C, Valdoz JC, Bickham BP, Knight CJ, Franks N, Chartrand N, Van Ry P, Christensen K, Nordin G, and Cook A. “Biocompatible PEGDA Resin for 3D Printing”. ACS Appl. Bio Mater. 2020 3: 2239-2244. 10.1021/acsabm.0c00055
Tissue Engineering and Disease Models: Articles by Harrick Plasma Users
- Tavana H. “Engineered 3D lung airway tree“. Patent US10777324B2 (2017).
- Park JH, Cho D, Lee J, Park JY, Ahn MJ, Nam IC, Kim SW, Lee JY, Lee JW, Park SH, and Yun BG. “Three dimensional tracheal substitute replacing respiratory organs and method of producing the same”. US20200163747A1 (2017).
- Burton TP. “Scaffolds and signals: design and development of a 3D printed bioreactor and electrospun polymer scaffolds for kidney tissue engineering”, The University of Edinburgh 2019. PhD thesis.
- Kumar A, Lau W, and Starly B. “Human Mesenchymal Stem Cells Expansion on Three-Dimensional (3D) Printed Poly-Styrene (PS) Scaffolds in a Perfusion Bioreactor”. Procedia CIRP 2017 65: 115-120. 10.1016/j.procir.2017.04.012
- Burgio F, Rimmer N, Pieles U, Buschmann J, and Beaufils-Hugot M. “Characterization and in ovo vascularisation of a 3D-printed hydroxyapatite scaffold with different extracellular matrix coatings under perfusion culture”. Biology Open 2018. 10.1242/bio.034488
- Vicente FN, Massou S, Wetzel F, Mehidi A, Strehle D, Leduc C, Voituriez R, Rossier O, Nassoy P, and Giannone G. “A micromechanical cell stretching device compatible with super-resolution microscopy and single protein tracking”. Protocol Exchange 2020. 10.21203/rs.3.pex-961/v1
Drug Delivery: Articles by Harrick Plasma Users
- Aghabaglou F. “Transdermal Drug Delivery Methods for Treatment of Chronic Skin Wounds”, University of Nebraska Lincoln 2020. PhD Thesis.
Composite Polymers: Articles by Harrick Plasma Users
- Patel BB, Walsh DJ, Kim DH, Kwok J, Lee B, Guironnet D, and Diao Y. “Tunable structural color of bottlebrush block copolymers through direct-write 3D printing from solution”. Science Advances 2020 6: eaaz7202. 10.1126/sciadv.aaz7202
- Jo Y, Kim JY, Kim S-Y, Seo Y-H, Jang K-S, Lee SY, Jung S, Ryu B-H, Kim H-S, Park J-U, Choi Y, and Jeong S. “3D-printable, highly conductive hybrid composites employing chemically-reinforced, complex dimensional fillers and thermoplastic triblock copolymers”. Nanoscale 2017 9: 5072-5084. 10.1039/C6NR09610G

This information has been sourced, reviewed and adapted from materials provided by Harrick Plasma.
For more information on this source, please visit Harrick Plasma.