Image Credit: https://fashionandtextiles.springeropen.com/articles/10.1186/s40691-021-00248-7
A newly developed 3D printed antenna for use in breast cancer treatment could make some procedures more efficient and comfortable.
According to the World Health Organization (WHO) in 2020 alone 2.3 million women were diagnosed with breast cancer and almost 700 thousand deaths resulted from this condition¹ which arises in the lining cells of the ducts or lobules in the glandular tissue of the breast.
There are currently an estimated 8 million women living with breast cancer who were diagnosed within the last five years, which represents around 64% of the total amount of cases globally. Fortunately, there are a number of treatment options available for breast cancer, including surgical removal, radiation therapy, and medication to treat microscopic cancer that has spread from the breast tumor through the blood.
In many cases, especially when caught early, these treatments can be effective in preventing cancer growth and thereby saving lives. But, as cancer survivors will attest, these methods are far from gentle, and receiving them can be an uncomfortable experience.
Assistance in this respect could be on the horizon for breast cancer patients, at least for those undergoing microwave breast hyperthermia procedures.
Scientists from North Carolina State University have developed a more comfortable radiation-receiving antenna that can be worn during the treatment. As well as being less bulky and more flexible than current devices, the receiver can be 3D printed, meaning it can be mapped to the shape of an individual patient's body, making it much more comfortable to wear.
That isn't the only advantage to the system, however. The team that designed it says that because their receiver allows adjustments so that its performance can be tuned to deliver varying levels of exposure.
The team's research is documented in a paper published in the International Journal of Interdisciplinary Research².
Making Microwave Breast Hyperthermia More Comfortable
Hyperthermia is a cancer treatment that uses high temperatures to treat the disease. It is often used in conjunction with other treatments and can be delivered locally or to the body as a whole, depending on the stage of the cancer being treated.
In microwave breast hyperthermia, breast temperature is elevated by a concentrated 'blast' of electromagnetic radiation — often in the microwave region of the electromagnetic spectrum — which impairs cancer cells by changing local blood flow, causing thermal damage and cellular death.
Even though the procedure is non-invasive, this technique hinges upon the use of extremely bulky and heavy antennas, which can cause patients significant discomfort during treatment sessions.
While wearable antennas have been suggested in the past, the implementation of such technology has been hampered by the fact that these devices would need in-built water cooling, making wearing them impractical. Textile antennas have also been suggested, but the fact that they would need to be individually manufactured to meet each patient's unique needs means that in practice such measures are unrealistic in terms of cost.
"3D-printed antennas could be a great alternative," says the North Carolina State University team. "In 3D printing, molten resin is deposited layer-by-layer to build an antenna structure. It is not an instantaneous task and takes time to 3D print. However, compared to the traditional fabrication of a textile product, 3D printing enables accurate and rapid manufacturing of custom designs at low cost, which is essential for a successful production."
3D Printing an Alternative Radiotherapy Antenna
Not only does the team's 3D printed antenna reduce discomfort, by investigating the relationship between the percentage of the structure that was solid volume and dialectic properties, the researchers also found a way of optimizing antenna performance.
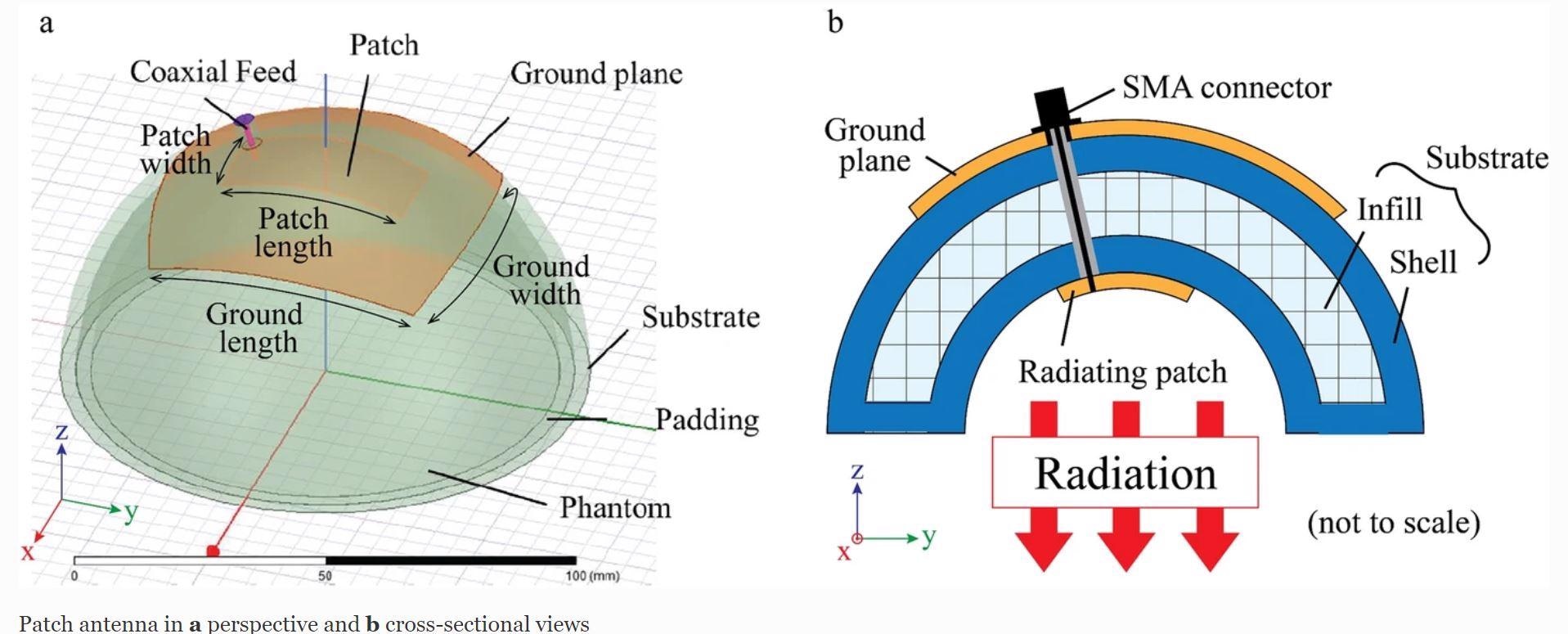
To test their system the team created three different models with a dual-head fused deposition modeling (FDM) printer, each of which had a different solid volume percentage — one at 40%, one at 70%, and the third filled to 100%.
Each model consisted of a conductive patch on a dialectic substrate and a 3 mm thick top layer that prevents the antenna from touching the patient directly. These prototypes were mounted upon a 'breast phantom' and were then exposed to electromagnetic simulations.
This led to the discovery of a linear relationship between the solid volume of the substrate and dialectic properties. This occurred without loss of heating efficacy with all the models producing temperature rises at 5 mm and 7 mm penetration of around 5.5⁰C and 3.3⁰C after 20 minutes of continuous exposure to radiation.
The North Carolina State University team points out that further work is needed on their antenna before it is ready for the next steps of its development. In particular, they say that a flexible filament with superior electric properties may be needed for a truly 3D printable antenna.
The next improvement recommended involves the testing of the device. As a real breast is made of innumerable components such as skin, fats, and blood vessels, the team's phantom breast is a poor substitute.
"For a further study, it is thus indispensable to consider a more realistic phantom," the researchers conclude.
References
1. ' Breast Cancer,' WHO, [https://www.who.int/news-room/fact-sheets/detail/breast-cancer]
2. Mukai.Y., Li. S., Suh. M., [2021], '3D-printed thermoplastic polyurethane for wearable breast hyperthermia,' International Journal of Interdisciplinary Research,[https://fashionandtextiles.springeropen.com/articles/10.1186/s40691-021-00248-7#auth-Yusuke-Mukai]
Disclaimer: The views expressed here are those of the author expressed in their private capacity and do not necessarily represent the views of AZoM.com Limited T/A AZoNetwork the owner and operator of this website. This disclaimer forms part of the Terms and conditions of use of this website.