Nov 13 2020
Scientists from the Skoltech Center for Design, Manufacturing, and Materials (CDMM) have developed a method for designing and manufacturing complex-shaped ceramic bone implants with a controllable porous structure, which largely enhances tissue fusion efficiency. Their research was published in the journal Applied Sciences.
Bone implant. Image Credit: Pavel Odinev / Skoltech
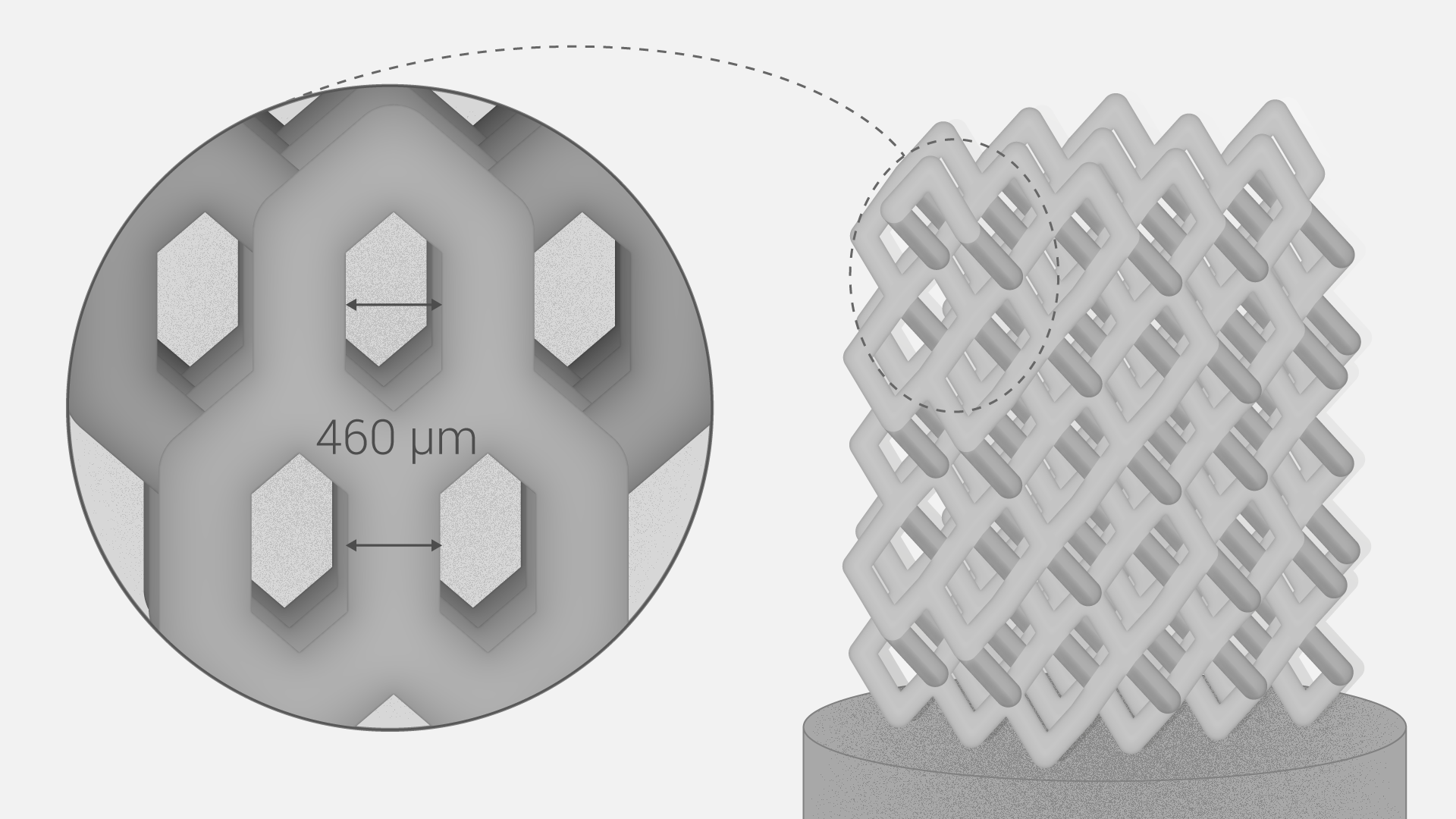
Ceramic materials are resistant to chemicals, mechanical stress, and wear, which makes them a perfect fit for bone implants that can be custom-made thanks to advanced 3D printing technology. Various porous structures are used to ensure effective cell growth around the implant.
For tissue fusion to be more efficient, the pores should have a size of several hundred microns, while the implants could be bigger than the pores by several orders of magnitude. In real life, an implant with a specific porous structure should be custom-designed in a very short time-frame. Conventional geometric modeling with the object representation limited to its surface does not work here due to the complex internal structure of the implant.
Skoltech scientists led by Professor Alexander Safonov modeled the implants using a Functional Representation (FRep) method developed by another Skoltech Professor, Alexander Pasko. “FRep modeling of microstructures has a wealth of advantages,” comments Evgenii Maltsev, a Research Scientist at Skoltech and a co-author of the paper. “First, FRep modeling always guarantees that the resulting model is correct, as opposed to the traditional polygonal representation in CAD systems where models are likely to have cracks or disjointed facets. Second, it ensures complete parametrization of the resulting microstructures and, therefore, high flexibility in the fast generation of variable 3D models. Third, it offers a diversity of tools for modeling various mesh structures.”
In their research, the scientists used the FRep method to design cylindrical implants and a cubic diamond cell to model the cellular microstructure. CDMM’s Additive Manufacturing Lab 3D-printed ceramic implants based on their design and tested them under axial compression.
Interestingly, the new method enables changing the porous structure so as to produce implants of different densities to accommodate the patients’ individual needs.