The phrase "cardiovascular disease" refers to any ailment that affects the cardiovascular system. It is frequently linked to fatty plaque in the arteries or atherosclerosis and an elevated risk of blood clots. Cardiovascular disease is the world’s leading cause of mortality, accounting for 45 percent of all fatalities in Europe (4 million people). Plasma-treated titanium stents can make a difference in this cardiovascular disease according to The International Journal of Molecular Science.
Study: Bio-Performance of Hydrothermally and Plasma-Treated Titanium: The New Generation of Vascular Stents. Image Credit: Floris Slooff/Shutterstock.com
New Treatment for CVD by Changing Titanium Surface
Over 60 million individuals in the EU are thought to be living with Cardiovascular disease, with over 13 million new cases diagnosed each year. SARS-CoV-2 infection exacerbates the strain of cardiovascular disease by causing cardiac injury, arrhythmia, heart failure, and pulmonary embolism, among other heart complications. The most widely accepted therapy for patients with CVD is the integration of a drug-eluting stent (DES).
Although DESs have shown to be better compared to bare-metal stents (BMSs) in terms of reducing neointimal hyperplasia, the first development of these devices also showed postponed endothelization as well as a higher likelihood of late stent thrombosis.
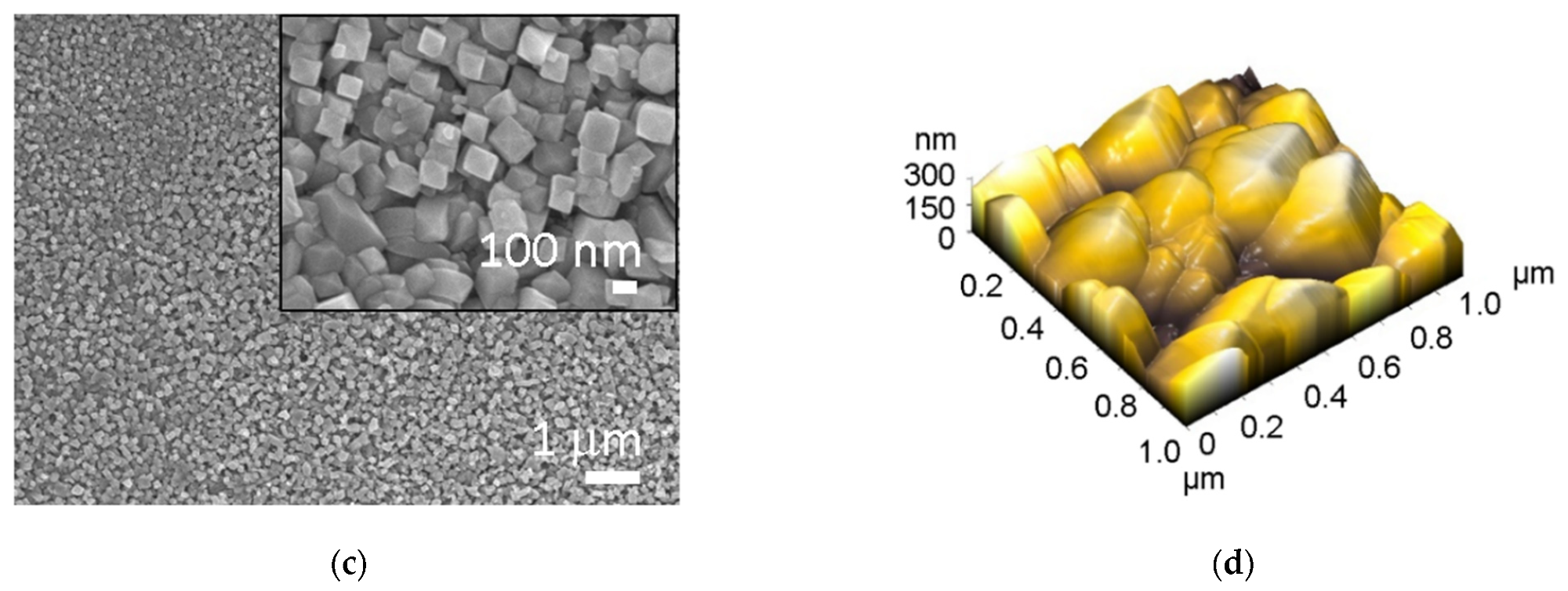
SEM and AFM images of: (a,b) untreated Ti foil (Ti), and (c,d) hydrothermally treated Ti (Ti HT), respectively. Image Credit: Bencina, M., et al., International Journal of Molecular Science
Various approaches can be used to nano-structuralize metallic surfaces. Such coatings can change the surface's physicochemical features, such as shape, roughness, wettability, and surface chemistry, which can impact how biological material interacts with it. The biological behavior of Ti surfaces that had been hydrothermally and plasma-treated was investigated.
The hydrothermal treatment allows for the creation of a homogenous nanostructured outer surface on Ti, according to the findings. There were no alterations in surface morphology or texture after plasma treatment, however there was an elevation in oxygen over all plasma-treated surfaces.
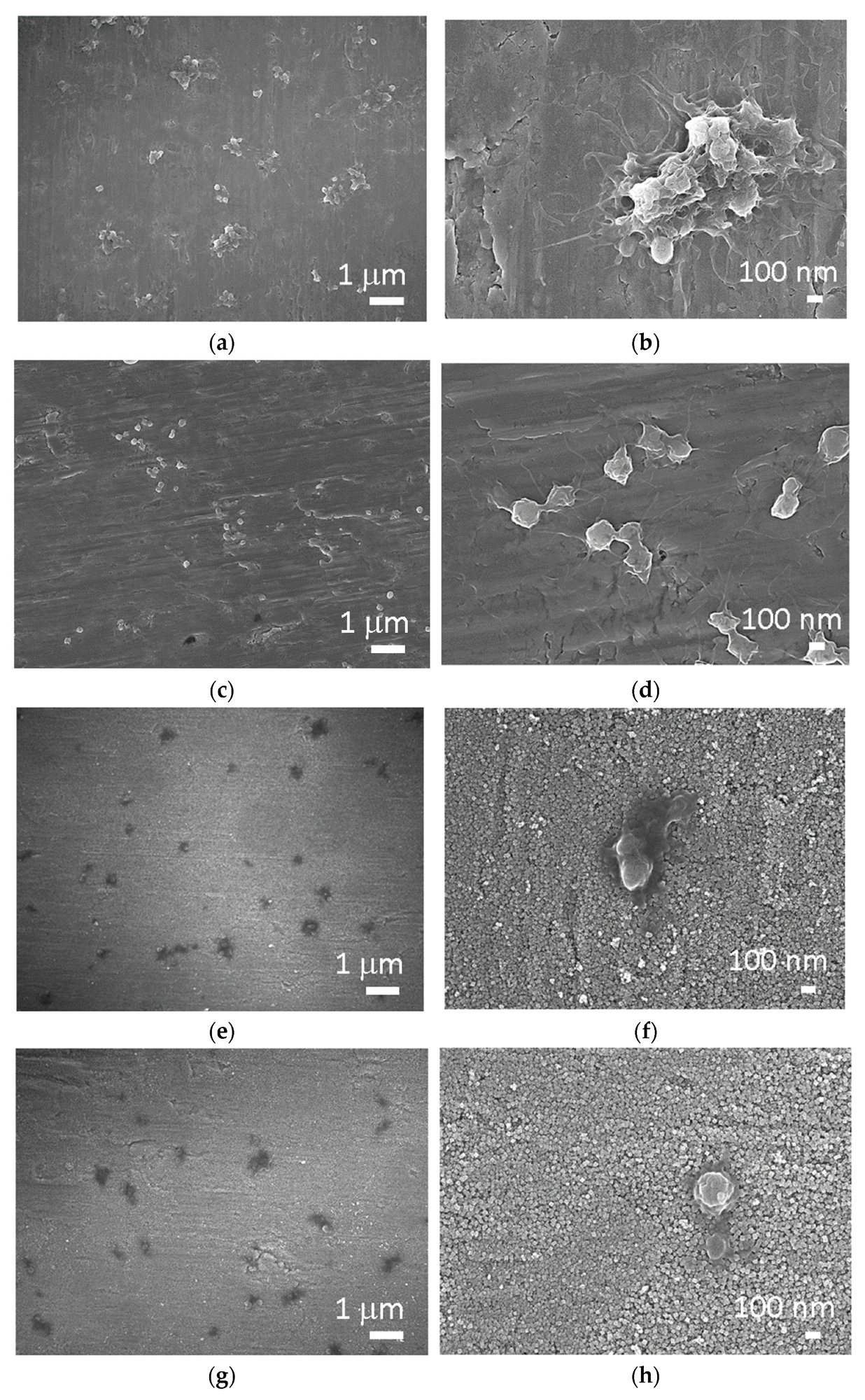
SEM images of (a,b) Ti foil, (c,d) Ti foil treated with plasma (Ti + P), (e,f) hydrothermally treated Ti foil (Ti HT) and (g,h) hydrothermally/plasma-treated Ti foil (Ti HT + P) after incubation with whole blood. Image Credit: Bencina, M., et al, International Journal of Molecular Science
Process of Nanostructured Titanium Oxide Surface
Because the surface was oxidized and carbon was eliminated, which is contaminated by reactive oxygen species, the primary difference in elemental composition was seen among plasma-treated and non-plasma-treated samples, with a considerable rise in oxygen and a reduction in carbon.
The changing physicochemical features of the Ti surface, especially shape, surface wettability, roughness, and chemical composition, have been found to impact the bio-performance of a material. The development of a nanostructured titanium oxide surface was achieved using a mixture of hydrothermal treatment and treatment with strongly active oxygen species (oxygen plasma therapy). Nanotopography has indeed been found to have an impact on blood platelet interaction.
The surfaces with the highest performance were nanostructured (TiO2 nanotubes) and treated with oxygen plasma. The presence of more oxygen on the material surface was shown to increase their hemocompatibility.
The future era of biodegradable polymer-coated stents was created to address the difficulties in CVD, particularly the prolonged inflammation of the artery wall produced by the presence of medications. Despite encouraging results in trials, late stent thrombus and dual antiplatelet medication were unavoidable.
Biodegradable vascular stents or scaffolds (BRS) have recently been produced and are now available on the market. These structures are not permanent, and their major benefit is that they provide temporary mechanical support in the vessel, which helps to avoid restenosis and vascular recoil.
Metal-based medical devices that come into contact with the bloodstream, such as vascular implants, nevertheless lack the required biocompatibility. Despite extensive study and significant advancements in metal surface alteration, metallic blood wired connections nevertheless pose a danger of surface-induced thrombosis and, as such, asrestenosis.
The greatest clinical risk following stent insertion is high platelet adhesion and activation, which is linked to stent thrombosis; platelets immediately stick to the site of damage, which is frequent in stenting operations, and begin to form a plug and blood clotting, which leads to artery blockage.
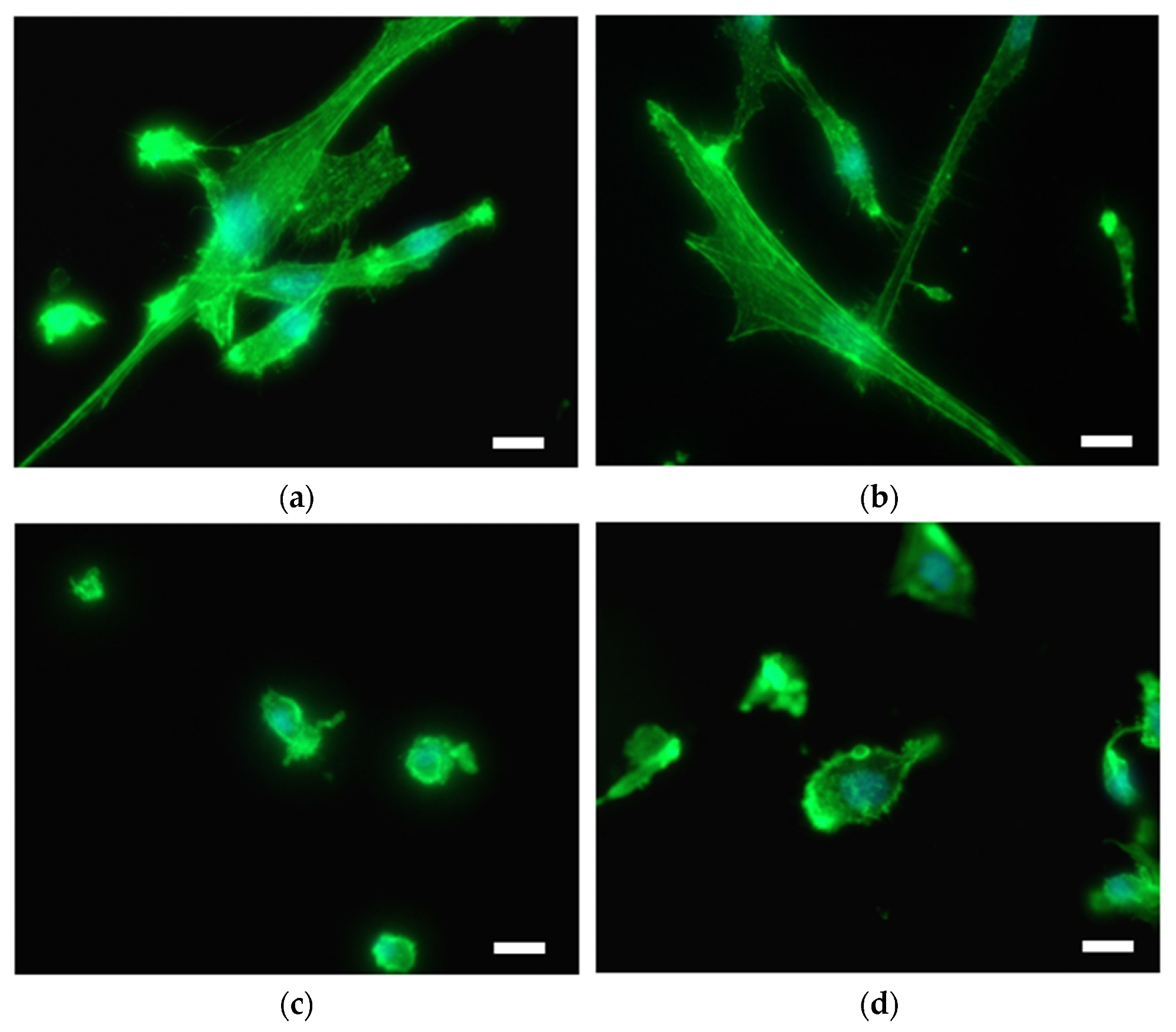
SMC on the surface of (a) Ti foil, (b) plasma-treated Ti foil (Ti + P), (c) hydrothermally treated Ti foil (Ti HT) and (d) hydrothermally/plasma-treated Ti foil (Ti HT + P), determined by immunofluorescent microscopy. F-actin is shown in green (Fluorescein Phalloidin). Nuclei are visualized with DAPI (blue color). Scale bar = 25 µm. Image Credit: Bencina, M., et al, International Journal of Molecular Science
Effects of Titanium Substrate
The effects of the Ti substrate's changed surface characteristics on interactions with coagulation factors and vascular cells are positive. The combination of nanostructurization and Titanium non-thermal plasma treatment resulted in a surface with improved morphological and chemical characteristics, making it ideal for use as vascular stents.
The metal surface has been changed using a mix of reactive oxygen and hydrothermal species treatments (non-thermal oxygen plasma). A nanostructured titanium oxide layer with increased oxygen concentration may be formed on the surface of a metal substrate using this approach.
It is believed that such surfaces will, to a lesser extent, elicit undesired thrombus formation in comparison to the untreated Ti foil. The surface that does not promote platelet aggregation is of significant importance for medical devices because the risk of thrombosis on such surfaces is reduced. The presence of more oxygen on the material surface was shown to increase their hemocompatibility.
References
Bencina, M., et al. 2021. Bio-Performance of Hydrothermally and Plasma-Treated Titanium: The New Generation of Vascular Stents. Published: 1 November 2021. https://www.mdpi.com/1422-0067/22/21/11858
Disclaimer: The views expressed here are those of the author expressed in their private capacity and do not necessarily represent the views of AZoM.com Limited T/A AZoNetwork the owner and operator of this website. This disclaimer forms part of the Terms and conditions of use of this website.