Mar 18 2016
Arthritis and sport-related injuries are a common occurrence in the elderly, athletes and others who experience severe pain as a result of damaged cartilage tissues. Scientists have now demonstrated how to use 3-D bioprinting to create cartilage tissues that could resolve this issue.
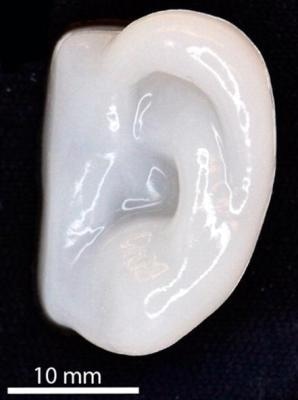 Scientists can 3D bioprint the shape of an ear using human cells that build up cartilage. (CREDIT Photo and Video credit: American Chemical Society)
Scientists can 3D bioprint the shape of an ear using human cells that build up cartilage. (CREDIT Photo and Video credit: American Chemical Society)
To produce the cartilage tissue the researchers completed the 3-D bioprinting with an ink containing human cells. This method has been successfully implemented in an in vivo mouse model. This innovation could help to develop accurately printed implants to cure damaged ears, noses, and knees in the future.
The study was presented at the 251st National Meeting & Exposition of the American Chemical Society (ACS). ACS is the world's largest scientific society. The meeting featured over 12,500 presentations on different topics of science.
Three-dimensional bioprinting is a disruptive technology and is expected to revolutionize tissue engineering and regenerative medicine. Our team's interest is in working with plastic surgeons to create cartilage to repair damage from injuries or cancer. We work with the ear and the nose, which are parts of the body that surgeons today have a hard time repairing. But hopefully, they'll one day be able to fix them with a 3-D printer and a bioink made out of a patient's own cells.
Paul Gatenholm, Ph.D, Wallenberg Wood Science Center
Gatenholm's research team at the Wallenberg Wood Science Center in Sweden are addressing this issue in a systematic and methodical way. The team first needs to develop an ink containing living human cells, which can retain its shape following printing. Materials that were printed previously would crumble into a shapeless pile.
Gatenholm's team successfully produced a bioink by combining polysaccharides with small cellulose fibrils and human chondrocytes, which build up cartilage tissue. Polysaccharides were obtained from brown algae, and cellulose fibrils from bacteria or wood. The group used this mixture to print living cells in certain shapes, like an ear that retained its shape after printing. The cells that were printed were also able to create cartilage in a lab dish.
But under in vitro conditions, we have to change the nutrient-filled liquid that the material sits in every other day and add growth factors. It's a very artificial environment.
Paul Gatenholm, Ph.D, Wallenberg Wood Science Center
The next stage was to shift the study from a laboratory dish to a living system. This was achieved by printing tissue samples and implanting them in mouse models, the cells successfully survived and created cartilage. Another obstacle in tissue engineering is to increase the cell number, for this the team combined human mesenchymal stem cells with human chondrocytes. Earlier studies have reported that primary cells are prompted by stem cells to proliferate in higher numbers than they would alone. Initial data, obtained from in vivo testing carried out over 60 days, revealed that the combination encourages the production of chondrocytes and cartilage.
According to Gatenholm, more studies would need to be performed prior to starting human trials. He has teamed up with a plastic surgeon to deal with issues related to regulatory and practical ethics. This would enable the most direct route.
Besides cartilage printing, Gatenholm's research group has partnered with a cosmetic company to create a 3D bioprinted human skin. In Europe, cosmetic firms are not allowed to test their products on animals and so they are hoping to utilize the 3D printed skin to test anti-wrinkling methods, makeup strategies, as well as ways to stop sun damage.