Apr 8 2014
With the new 3D Bioprinter, the research group of Professor Paul Gatenholm at the Department of Chemical and Biological Engineering exploits new possibilities of tissue engineering and organ regeneration.
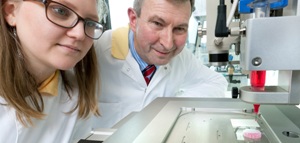
Professor Paul Gatenholm's research has gained a lot of attention lately, both in newspapers and on television. We contacted him for a quick interview!
The television newscast can be viewed here (in Swedish)
Read the article in Ny Teknik here (in Swedish)
How does bioprinting work?
3D Bioprinter is a robotic arm which can dispense fluids with high resolution. We talk about 10 micrometers. Bioprinter has several printing heads with which it can dispense high viscous suspensions, extrude hydrogel and dispense cell suspension. It is designed to work in sterile environment so it can handle human cells in the same operation when the hydrogel which will support human cells will be dispensed. It can handle several different cell types at the same time. 3D Bioprinter is thus able to produce a scaffold with microarchitecture corresponding to microstructure of tissue which is going to be reproduced.
How can it be used in Life science research?
We can produce model tissues which will function as the whole organ. Those model organs are called organoids. We have prepared model of adipose tissue which can be used to screen drugs for treatment of obesity. The challenging organ is liver and we are working to prepare miniature liver using human hepatocytes. The advantage is that the cells can be used from patient who has disease and thus lead to development of patient specific drugs. The big advantage is also to omit animal study and in early stage test on human organoid without entering clinical trials.
What do you think is the next advancement in technology that will further help the development of artificial organs?
We are working together with Sahlgrenska and companies within our region with iPSC (induced pluripotent stem cells) derived from adult cells. These cells can be proliferated and differentiated to any cell type. We are currently working with iPSC cells derived from cartilage which are reprogrammed to iPSC and we study differentiation to chondrocytes to be able to create model of osteoarthrisis but in long term to be able to repair cartilage.
How can blood vessels be made and incorporated when manufacturing more complex tissues?
Vascularization is crucial when biofabricating of larger organs or tissue which demands oxygen and removal of waste products. One way to introduce blood vessels is to print with sacrificial polymer and then remove it. Then to inject endothelial cells in created cavities.
What are the major obstacles for printing a functional heart?
The major challenge will be to handle the cells and provide them with right environment. We need to learn more about microarchitecture of heart but also to develop new materials which can host cardiac cells. Then it must be clear that 3D Bioprinter is not printing final tissue or organ. It is building the scaffold and seeding cells in right place. Such cell-laden construct has to be removed to incubator and in most cases into bioreactor to be converted into tissue or organ. This process can take several weeks.
What is the next step for your research group?
We are focusing on developing nanocellulose as Bioink. Our group has long experience of nanocellulose implants and scaffolds for tissue engineering. With 3D Bioprinting we are challanged with needs to control rheology during printing process and solidification of hydrogel. Then we need to be able to handle cells at the same time. Lot of coordination of material science, cell biology and engineering.