Mar 29 2019
Bioscientists are advancing toward 3D-printed artificial tissues to help treat bone and cartilage usually damaged in sports-related injuries to elbows, knees, and ankles.
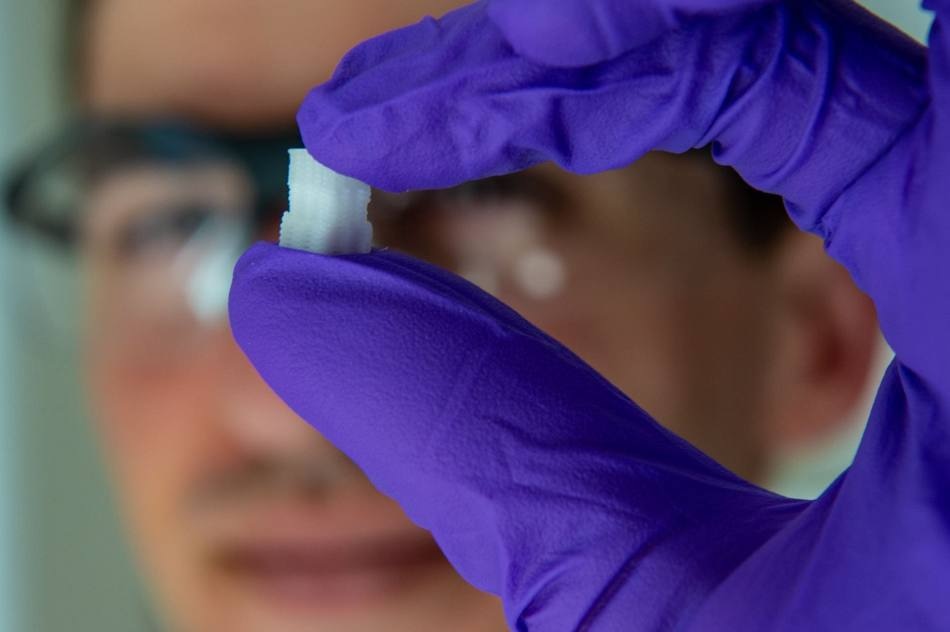 Rice University graduate student Sean Bittner holds a 3D-printed scaffold created to help heal osteochondral injuries. The initial study is a proof-of-concept to see if printed structures can mimic the gradual transition from smooth, compressible cartilage to hard bone at the end of long bones. (Image credit: Jeff Fitlow)
Rice University graduate student Sean Bittner holds a 3D-printed scaffold created to help heal osteochondral injuries. The initial study is a proof-of-concept to see if printed structures can mimic the gradual transition from smooth, compressible cartilage to hard bone at the end of long bones. (Image credit: Jeff Fitlow)
Researchers at Rice University and the University of Maryland reported that they have successfully engineered scaffolds for the first time that mimic the physical characteristics of osteochondral tissue, which is essentially hard bone underneath a compressible layer of cartilage that appears as the smooth surface on the ends of long bones.
Damages to these bones, from tiny cracks to portions that detach, can be hurting and usually end athletes’ careers in their tracks. Furthermore, osteochondral injuries can result in disabling arthritis.
Due to the gradient nature of cartilage-into-bone and its porosity, it has been challenging to reproduce osteochondral tissue in the lab; however, researchers at Rice University headed by bioengineer Antonios Mikos and graduate student Sean Bittner have employed 3D printing to engineer what they believe will be an ideal material for implantation in the due course.
Their results are published in Acta Biomaterialia.
Athletes are disproportionately affected by these injuries, but they can affect everybody. I think this will be a powerful tool to help people with common sports injuries.
Sean Bittner, Third-Year Bioengineering Graduate Student, Rice University
Bittner is also a National Science Foundation fellow and lead author of the paper.
The solution is replicating the tissue that transforms slowly from cartilage (chondral tissue) at the surface to bone (osteo) beneath. The Biomaterials Lab at Rice printed a scaffold using custom mixtures of a polymer for the former and a ceramic for the latter with embedded pores that would enable the patient’s own cells and blood vessels to penetrate the implant, ultimately enabling it to become a part of the natural bone and cartilage.
“For the most part, the composition will be the same from patient to patient,” noted Bittner. “There’s porosity included so vasculature can grow in from the native bone. We don’t have to fabricate the blood vessels ourselves.”
The future of the project will involve understanding how to print an osteochondral implant that appropriately fits the patient and enables the porous implant to grow into and join with the bone and cartilage.
Mikos said the partnership is a significant early success for the Center for Engineering Complex Tissues (CECT), a National Institutes of Health center at Maryland, Rice, and the Wake Forest School of Medicine producing bioprinting tools to focus on fundamental scientific questions and convert new knowledge into clinical practice.
In that context, what we’ve done here is impactful and may lead to new regenerative medicine solutions.
Antonios Mikos, Bioengineer, Rice University
Co-authors of the paper include Rice graduate student Brandon Smith, postdoctoral researcher Luis Diaz-Gomez, undergraduate Carrigan Hudgins, Anthony Melchiorri, associate director of the Biomaterials Lab, and David Scott, the Noah Harding Professor of Statistics; and John Fisher, CECT director and Fischell Family Distinguished Professor and chair of the University of Maryland’s Fischell Department of Bioengineering. Mikos is the Louis Calder Professor of Bioengineering and a professor of chemical and biomolecular engineering, of chemistry, and of materials science and nanoengineering.
The work was supported by the National Institutes of Health and the RegenMed Development Organization.