A paper recently published in the journal ACS Applied Bio Materials reviewed the potential and current applications of polycaprolactone (PCL) for heart regeneration therapy.
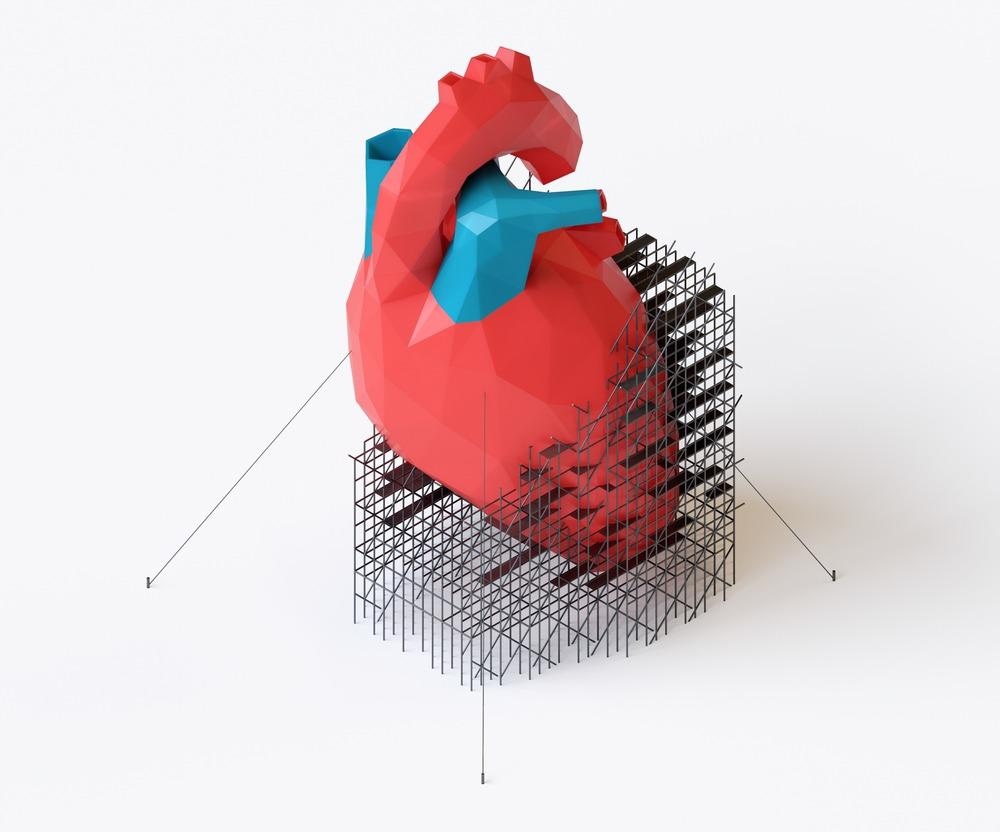
Study: Current Applications of Polycaprolactone as a Scaffold Material for Heart Regeneration. Image Credit: eranicle/Shutterstock.com
Background
Heart failure (HF) remains the major cause of death across the world despite significant advancements in treatments for cardiovascular diseases (CVDs). The loss of functioning cardiomyocytes (CM) is primarily responsible for CVD progression. Surgical implantation of a cellularized patch on a diseased heart is one of the leading strategies to reengineer cardiac function through contractile tissue regeneration and reduce the effects of damaged tissues on heart longevity and function.
Tissue scaffolds can be used to recapitulate the structural and mechanical environment of the native heart in the diseased heart to promote engineered myocardium function and contractility. PCL scaffolds can mimic the structure and mechanics of the native heart.
These scaffolds are investigated for myocardium regeneration due to their simple fabrication, biodegradability, and desirable biocompatible, chemical, and mechanical properties. Thus, PCL scaffolds are suitable for reengineering and regenerating the function of the heart after injury or disease.
In this review, researchers focused on the application of PCL as a tissue scaffold, specifically in myocardium regeneration and repair, and a roadmap for clinical translation of this PCL-based technology.
The Ability of PCL Scaffolds to Recapitulate the Mechanics of Native Myocardium
The ability of the scaffolds to withstand repetitive and high mechanical loading and the anisotropy and elasticity of the structure must be considered while designing engineered cardiac tissues as a regenerative therapy after cardiac disease/injury. PCL is a mechanically strong polymer with Young’s modulus (YM) of 330−360 MPa and adequate tensile strength between 25 and 43 MPa.
Although PCL is not considered to be a mechanically suitable scaffold for soft tissues such as myocardium due to its high YM, the development of new strategies to make PCL better suited for heart wall implantation has significantly increased the potential of the polymer for cardiac applications.
In cardiac tissues, PCL is typically applied in the form of fibrous scaffolds that leave significant space for cell proliferation and infiltration, leading to an increased cross-sectional area without added mechanical reinforcement, which substantially decreases the YM of many scaffolds compared to the bulk polymer. Additionally, hydrogels are typically utilized to improve cell proliferation and embed these scaffolds, which further decreases their YM.
The biodegradable polymer fully degrades within two to three years. However, the degradation of mechanical properties of PCL scaffolds, such as YM, occurs within the first few months. In vitro studies demonstrated that the YM decreased by 60% and 40% within four and two months, respectively, due to hydrolytic degradation.
PCL Scaffold Biofabrication Methods
PCL can be easily dissolved in organic solvents such as chloroform and acetone and has a low melting point. Thus, the physical features of PCL can be modified using large-scale biomanufacturing processes. Wet spinning, three-dimensional (3D) printing, and electrospinning methods can be used to change the properties and geometry of PCL.
The electrospinning process is the most common PCL scaffold fabrication technique. In this process, the PCL fiber diameter can be altered by varying the humidity and temperature, presence of bending polymers, applied voltage, and solution concentration. Electrospinning is used extensively for the fabrication of nanoscale PCL fibers owing to its ease of fiber production and adaptability of parameters.
3D printing is a more recent method for PCL scaffold fabrication. The 3D composition and structure of the fabricated PCL scaffold can be controlled precisely in this method through computer-aided design.
Although wet spinning is commonly used for biological fiber preparation, the method, specifically its subtype gravity spinning, has gained attention for polymer fiber fabrication. The lower risk of inconsistency owing to environmental conditions is the major advantage of wet spinning over the electrospinning method. However, the PCL fibers produced through this method have large diameters that can prolong the degradation time and affect cell infiltration.
Physical and Chemical Modifications Influence PCL Properties
Bulk modifications can lead to chemical changes to the entire PCL scaffold. These modifications can be used to promote cell infiltration, modulate the mechanics, and enhance the electrical conductivity of the scaffolds. Carbon nanotubes and silk fibroin are often used as blending materials to change the PCL mechanics through bulk modification.
Additionally, PCL can be used in composite systems, such as a layered scaffold. For instance, unblended PCL can be embedded within a hydrogel to fabricate a composite scaffold. The addition of hydrogel can bring down the high YM value in PCL fibers closer to the value of healthy native myocardium without decreasing the PCL fiber strength.
Surface functionalization and modification of a PCL scaffold surface by changing the surface attributes, such as the surface porosity, energy, and charge, can enhance cell proliferation and adhesion.
PCL Scaffolds can Modulate Biological Interaction
In cardiac tissues, the CM alignment is critical to the force-generation capabilities of myocardial tissue. CM maturation, overall function, and alignment are the three definitive indicators of a successful myocardial scaffold.
Blending PCL with aligned conductive polymers can create electrical anisotropy within the PCL scaffold. The method can improve the expression of the mature CM markers and human-induced pluripotent stem cell-derived CM (hiPSC-CM) signaling.
PCL is nonimmunogenic as PCL implantation shows little or no inflammation in the body. Different in vivo studies have confirmed that PCL implantation generates no inflammatory response.
Moreover, a significant decrease in the production of inflammatory cytokines, such as transforming growth factor-beta-1 (TGF-ß1) and interleukin 6 (IL-6), was observed in a study when a gelatin sheath was wrapped around the fibrous PCL core.
Current Advancements of PCL in Cardiac Tissue Engineering (CTE)
CM attachment is the first consideration of PCL scaffolds used in vitro in the field of CTE. Several methods, such as chemical modifications and bulk modifications, were utilized to promote chemical attachment and infiltration of CM to PCL scaffolds. Chemical modification with sodium hydroxide significantly improved the hydrophilicity of PCL scaffolds, leading to greater CM attachment.
Similarly, the mechanical stiffness of PCL was decreased using several techniques, such as creating composite and blended scaffolds or modulating the PCL biofabrication technique. For instance, the YM of a PCL scaffold was decreased successfully by fabricating a porous PCL scaffold using a selective laser sintering technique.
The mechanical and structural anisotropy of the PCL scaffolds were tuned using more complex techniques. For instance, parallel, 90o, 60o, and 30o electrospun PCL fibers were engineered to tune the anisotropy of the PCL scaffolds.
In Vivo Testing of PCL Scaffolds to Assess Cardiac Function
In a study, a mesenchymal stem cell (MSC)-seeded poly(lactide-co-ε-caprolactone) scaffold was utilized on a cryo-injury model of myocardial infarction in rodents. The study findings indicated that the infarct area decreased and left ventricular ejection fraction increased significantly in the implant group compared to the saline injection controls.
Cardiac magnetic resonance imaging (MRI) has emerged as a versatile, noninvasive, and accurate method for in vivo investigation of cardiac function and structure to assess the effectiveness of PCL-based therapies.
Clinical Translation of PCL-based Regenerative Therapy in Cardiac Engineering
To achieve clinical translation of PCL-based regenerative therapy in cardiac engineering, studies based on a comprehensive design that can target several requirements of a successful cardiac tissue scaffold are necessary.
The design must focus on ensuring electromechanical integration between host myocardium and engineered tissues, promoting vascularization of native and engineered tissues, providing mechanical reinforcement to both native and engineered tissue, and promoting cell function and attachment.
Conclusion
To summarize, PCL has great potential in cardiac engineering due to its versatility, biodegradability, and mechanical strength. In the future, PCL can be used for in vitro modeling, drug delivery, and engineered cardiac tissue maturation and can provide anisotropic support to the heart after disease/injury. However, more research is required to overcome certain challenges such as tissue vascularization and CM immaturity before developing a cellularized clinical treatment for heart failure.
More from AZoM: Considering the Behavior of Doped SrTiO3 Ceramics
Disclaimer: The views expressed here are those of the author expressed in their private capacity and do not necessarily represent the views of AZoM.com Limited T/A AZoNetwork the owner and operator of this website. This disclaimer forms part of the Terms and conditions of use of this website.
Source:
Coulombe, K. L. K., Dwyer, K. D., Schmitt, P. R. Current Applications of Polycaprolactone as a Scaffold Material for Heart Regeneration. ACS Applied Bio Materials 2022. https://pubs.acs.org/doi/10.1021/acsabm.2c00174