A research team comprising Thomas Webster and Lijuan Zhang from the Brown University has developed an implant that has a nanoscale ‘bed-of-nails’ surface, which prevents the survival and growth of cancerous cells.
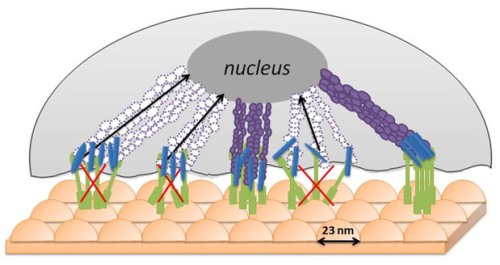 A bumpy “bed of nails” surface does not allow cancerous cells to gather the nutrients they need to thrive — possibly because cancerous cells are stiffer and less flexible than normal cells, which can manage the bumps and thrive. Credit: Webster Lab/Brown University
A bumpy “bed of nails” surface does not allow cancerous cells to gather the nutrients they need to thrive — possibly because cancerous cells are stiffer and less flexible than normal cells, which can manage the bumps and thrive. Credit: Webster Lab/Brown University
The nanoscale modifications on the surface of the implant shrink the blood-vessel network that forms the basis of cancer cells, while welcoming healthy breast cells. Webster informed that the team has produced an implant with novel features, which can limit the functions of cancer cells without the use of cancer cell-destroying processes such as radiation and chemotherapeutics.
In this study, the research team wanted to redesign an implant to be utilized in breast reconstruction surgery. The team fabricated a cast over a glass plate utilizing polystyrene beads having a diameter of 23 nm and polylactic-co-glycolic acid (PLGA), a FDA-approved biodegradable polymer. The resulting product is an implant with a surface covered with adjoining peaks of height of 23 nm. The team also fabricated PLGA implant surfaces with 300 and 400-nm pimples for comparison.
After one day of laboratory experiments, the team observed that the production of VEGF, a protein, which is the basis of endothelial breast-cancer cells, was decreased by 15% by the 23-nm-pimple surface when compared to a surface without any surface modification. The 23-nm-peak surface’s ability to reduce the VEGF concentration was also better than that of 300 and 400-nm-peak implants.
Although, the reason is not clear for the superior performance of the 23-nm implant surface in repelling breast-cancer cells, Webster believes that the bumpy surface does not allow the malignant breast cells to completely wrap themselves around the curved shapes, preventing them from consuming the life-sustaining nutrients. He added that surface peaks below 23 nm may perform even better. However, polystyrene beads of a diameter below 23 nm are not yet available. The team also discovered that 23-nm semispherical surface increased the production of healthy endothelial breast cells by 15% when compared to a normal surface in lab tests after one day.
The research team’s next step is to study the reason behind the nanomodified surfaces’ ability to repel malignant breast cells, to fabricate surface features that produce better results, and to identify the possibility of using other materials.